During a trip to the US Med Tech conference Advamed last October, Timothy Allan heard the US Food and Drug Administration (FDA) and Centre for Devices and Radiological Health (CRDH) discuss developments of medical device evaluation strategies and how computational modelling and simulation is accelerating medical device development.
Finite element analysis (FEA) is a computational process of dividing complex problems into many small sub-functions and solving each in relation to each other. This is typically used to analyse the stress and strain distribution through a part before it is manufactured. The use cycle of a part can be simulated within the software allowing for design optimisation based on how the part performs under stress. FEA is the interpretation of this complex information into useful information.
The FDA has been accepting computational data for some years now as part of a submission package for medical device acceptance. The other evaluation models include animal, bench, and human testing. The FDA have seen an increasing trend in simulation based submissions for medical devices, as engineers are achieving increasingly accurate levels of precision when evaluating device functionality previously not possible in physical testing.
A company that developed a range of intervertebral body-fusion devices (IBFD) – artificial spinal vertebrate for spinal injuries – were faced with FDA testing costing US$1.2M for the product range. As an alternative strategy, FEA was used to prove that if the weakest variant in the range (in FDA test terms) would pass the physical testing, the stronger variants would also. The FEA process in this case saved enormous costs and time to market.
We know through our work in the aerospace industry that a similar compliance method is used for testing of aircraft parts. Boeing operates ‘allowables’ testing, where mechanical assurance of materials is proven through statistical analysis. This tolerance data of material performance is then inputted into FEA models of aircraft parts. If the part passes in the FEA testing at the lowest threshold, the part is accepted. Physical engineering static testing is only performed for components that are substantiated by new or unproven analysis methods. This approach can radically speed up development times (compliance can be demonstrated before parts are manufactured) and reduce significant static load testing.
Bausch & Lomb, the contact lens and eye health specialists, are also employing FEA in a biomedical context to develop highly flexible intraocular lenses (IOL). The highly flexible hydrophobic acrylics and silicones allow tiny 1mm surgical incisions into the eye for IOL fitment – halving the previous incision length and reducing patient recovery time. This is however “like trying to suck a Frisbee through a vacuum,” says Robert Stupplebeen, a B&L Design Engineer and Analyst, as the lens has to fold to pass through the incision hole. The lens and applicator was modelled in FEA software then analysed to measure strain on the lens and visualise the deformation of the lens as it passes through the microscopic applicator channel into the eye. The FEA model was compared and calibrated against physical test data – peak strain measurements correlated to previously experienced real-world failures points. The FEA process provided information that was previously unavailable to B&L, such as the stresses applied to the lens by the applicator. This simulation approach has resulted in higher assurance of what will work when production is committed and failure modes mitigated in use.
It is important to note that FEA is not a substitute for bench or human testing in the entirety. FEA models should, where possible, be calibrated against physical data derived from bench testing. This will mitigate risk upstream during in vivo (in living organism) testing.
FEA has proven to be a valuable tool for medical device development that can reduce time to market and hefty physical test costs. Also proven by the B&L example, FEA can unlock information previously unattainable by traditional physical test methods. In our world, this derives valuable insights that can lead to breakthrough product ideas. The acceptance of FEA in compliance submission adds further weight to use of simulation.
Recognising the opportunity for medical device developments we connected the dots and while Tim was hearing B&L present their intraocular FEA research at Advamed we had a funding application in progress to support an FEA research project. The MBIE-supported programme explored the use of computational modelling and simulation in the development of a biomechanical test apparatus for the hip protector we took to market in 2011.
The whitepaper released from this study describes how we used FEA to develop a surrogate soft tissue model used within an apparatus to test hip protector devices.
FEA in Biomedical Hip Protector Research
Background
Our intensive test-driven development programme was the biomechanical test apparatus that simulated the impact event (impact energy) of an elderly person’s fall: 28Kg from 0.5m impacts a hip protector device overlying a surrogate soft tissue and proximal femur model. A specific spring represents the mechanical compliance of the pelvis during a fall and integrated piezoelectric sensor measures impact and attenuated force (from beneath the hip protector device). The apparatus was built to a specification developed by the International Hip Protection Research Group (IHPRG) – a consensus group of international falls and biomechanical experts. We recognised that the surrogate model representing the soft tissues surrounding the hip bone was a key component in the test system that strongly affects the performance of the hip protector device being tested. The specification for this component was largely underdeveloped and opinion continues to evolve in the biomechanical fields about what artificial material best represents the mechanical behaviour of soft tissues.
Our Aims
Our Process
Establishing links with the Auckland Bioengineering Institute of Auckland University, Matthew Davison joined the Locus team for 10 weeks during the summer before the final year of his Biomedical degree to tackle the MBIE funded project. Read a humorous account of his experience here.
Physiological research of the hip region identified three key components that form the hip region soft tissues: skin (epidermis and dermis), fat (hypodermis), and muscle. In order to simulate these components in an FEA package, the basic Young’s, bulk, and shear modulus mechanical characteristics had to be determined. In FEA terms biological materials are hyperelastic meaning they do not perform like standard non-biological components but rather demonstrate non-linear, viscoelastic characteristics instead. Hyperelastic equations derived the coefficients for the three components. The research identified that the collagen fibres in the dermis layer creates an anisotropic property where the material stiffness increases when stressed in the direction of the fibres. Additional variables such as hydration, muscle growth, muscle fibre types, fat volumes, and location on the body illustrate just how complex biology materials are for simulation.
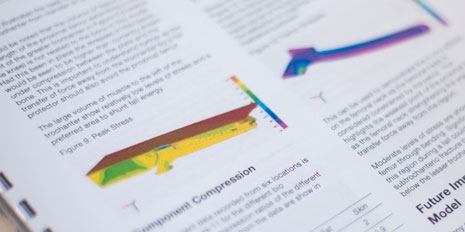
FEMAP with NX NASTRAN FEA software was used to simulate the soft tissue model and develop schematic understanding of how impact forces are transmitted into the hip’s soft tissues. The first iteration of the FE model was simplified with a view to increase complexity in future models. The FEA process is complex with vast amounts of variables and conditions required to represent real-world phenomena. In the FEA world complexity is correlated to computational time – one model took over 70 hours to analyse on a Quad Intel Xeon Processor machine (quick for most).
Materials research investigated artificial material that would better mimic the mechanical properties of soft tissue derived from the research. Platinum cured silicone was identified as the closet match due to its viscoelastic properties and relative stiffness. A three layered (skin, fat, and muscle) physical test model was developed for use on the impact test rig and evaluated against the existing polyethylene foam model.
Outcomes
The FE analysis proved to be an immensely valuable research tool deriving insights into how fall energy propagates through the tissues and bones, the stresses in the femoral neck (hip fracture location), the stress through the proximal femur (upper thigh bone), and compressibility of the softer fat layers versus the tougher skin and muscle. As a pure visualisation tool, having the ability to dissect the model and see the forces inside the hip region was invaluable and will undoubtedly shape the next generation hip protector for Delloch.
View the whitepaper to read the full study:
The need for standard approaches to simulation is becoming increasingly important as FEA moves from an exploratory research tool into an accepted compliance method. There are calls for standardised reporting approaches for FEA so the model structure and conditions are documented and visible for assessment and reproducibility. For researchers this approach will have further benefit as shared learning and consistent test beds for analysis. One of the most significant and ambitious shared learning simulation projects is underway and gathering momentum. The Physiome Project - “physio” (life) + “ome” (as a whole) - has the bold vision of developing a computational framework to model the complete virtual physiological human.
The Human Genome Project, that successfully mapped a complete genome sequence over 13 years, has set the benchmark for the wider-reaching, umbrella Physiome Project/Virtual Physiological Human Project. Large databases of physiological, anatomical, and pathological data are being combined on a worldwide effort to form predictive models of the human body to further clinical understanding of the entire integrated system from cells to organs. Where computational modelling is helping develop medical devices today, it is predicted that in five years in-silico (computer simulations) models will be trialling pharmaceutical drugs as well.
As Professor Marco Viceconti says in his TED Talk, this is the future of healthcare. Healthcare professionals will be able input patient specific data into the model and output predictive health results, develop personalised medicine, and trial virtual surgical procedures.
Comments
Post new comment